The Science of Sunlight
A corona mass ejection erupts from our sun on August 31, 2012 - photo provided by NASA.
Over 1 billion people worldwide are estimated to be vitamin D deficient, a statistic largely attributed to our modern avoidance of sunlight. Some scientists have even described vitamin D deficiency as a pandemic, suggesting that up to 50% of the global population may be affected. While much attention has been given to the risks of sun exposure, such as skin cancer, the potential dangers of inadequate sunlight exposure have often been overlooked. Yet sunlight plays a crucial role in optimizing health, particularly through its impact on vitamin D production and other biological processes. Understanding how light affects your body and learning to safely maximize exposure to sunlight can have profound benefits for your well-being.
But first, what is light? Light surrounds us every day and is scientifically referred to as electromagnetic radiation (EMR). It consists of massless particles called photons, which carry energy and momentum based on their wavelength and frequency. The electromagnetic spectrum encompasses all possible wavelengths of EMR, including gamma rays, x-rays, ultraviolet (UV) rays, visible light, infrared (IR), and radio waves. The visible light spectrum, which ranges from 380 nm to 780 nm, represents the small portion of this spectrum that the human eye can perceive. We see these wavelengths as colors—blue, red, yellow, and green—though most wavelengths remain invisible to us. Each type of light interacts with the body in unique ways, making light exposure an essential factor in health optimization.What happens when light comes into contact with matter? Matter is made up of atoms, ions, and molecules, each containing electrons. These electrons vibrate at specific frequencies due to their electrical charge. When a light wave interacts with an atom and is absorbed, the atom's electrons begin to oscillate in harmony with the light's electromagnetic frequency. This phenomenon, known as wave oscillation, can be likened to tuning a musical instrument, where precise vibrations create resonance. As the initial atom's electrons vibrate, neighboring atoms are also set into motion, generating thermal energy, or heat.
Light enters the human body primarily through two key pathways: the retina and the skin. While the absorption of light reduces its energy, it also triggers vital biological processes. For the majority of human history, sunlight has been our main light source, shaping our physiology to not only respond to its specific frequencies but to depend on them for survival. From regulating circadian rhythms to synthesizing essential compounds like vitamin D, sunlight has been fundamental to human health.
Check out this video for helpful visuals of the electromagnetic spectrum:
Skin in the Game
Figure 1. from Vitamin D: The “Sunshine” Vitamin
Unlike other essential vitamins that are primarily obtained through diet, vitamin D3 is unique in that it is primarily synthesized in the skin through a photosynthetic reaction triggered by ultraviolet B rays (UVB, between 290–315 nm) from sunlight. This process begins with 7-dehydrocholesterol, a cholesterol precursor located in the epidermal layer of the skin. When UVB rays penetrate the skin, they convert 7-dehydrocholesterol into previtamin D3, effectively allowing the skin to absorb this electromagnetic energy. Interestingly, only about 15% of 7-dehydrocholesterol converts to previtamin D3 after sun exposure, making it impossible to overdose on vitamin D3 from sunlight alone. The remainder transforms into other compounds, such as lumisterol3 and tachysterol3, or reverts back to 7-dehydrocholesterol.
Once formed, previtamin D3 enters the bloodstream, binds to plasma proteins, and undergoes two hydroxylation reactions—first in the liver and then in the kidneys—to become the active form of vitamin D3 (25-hydroxyvitamin D). However, many cells and organs, including the skin itself, possess vitamin D receptors (VDR) and have the capacity to produce the bioactive version of vitamin D3 (1,25-dihydroxyvitamin D). Remarkably, most of the vitamin D3 produced in the skin remains in the epidermis, even after washing with soap and water immediately following sunlight exposure.
Ultraviolet A rays (UVA, 315–400 nm) also play a pivotal role in skin physiology. When UVA rays interact with the skin, they trigger the production of nitric oxide (NO), a molecule with numerous therapeutic benefits. NO acts as a potent vasodilator, relaxing and widening blood vessels, which enhances the transportation of vitamin D, previtamin D, and their metabolites throughout the body. This process creates a feedback loop: optimized levels of vitamin D stimulate further NO production in the skin, creating a synergistic relationship between sunlight exposure, NO, and vitamin D synthesis.
Additionally, NO plays a crucial role in the absorption and utilization of UV and infrared (IR) light. Since UV light penetrates less than a millimeter into the skin, the circulatory system must deliver hemoglobin to these superficial layers for light absorption. NO facilitates this by promoting vasodilation, resulting in a reddish appearance on the skin after sun exposure. However, sensitivity to this process varies depending on factors such as geographic location and lifestyle. Individuals living in northern latitudes or spending much of their time indoors may be more prone to acute toxic reactions, such as prostaglandin and cytokine release during vasodilation, when suddenly exposed to high levels of UV light. Conversely, those living closer to the equator or spending more time outdoors tend to develop greater resistance to these effects.
Melanin, Latitude, & Altitude
Robby, standing on the Equator in rural Uganda.
Only about 1% of UVB radiation from the sun reaches the Earth’s surface—even at noon during summer months—because most of it is absorbed by the stratospheric ozone layer. However, the ozone layer is not the only protection nature has devised against UV radiation. Melanin, a pigment in the skin, plays a pivotal role in managing UV radiation exposure by absorbing light within the spectrum of 290–700 nm. This dual role of protection and regulation underscores melanin's evolutionary importance.
All humans have roughly the same number of melanocytes—the cells responsible for producing melanin. However, the amount of melanin synthesized varies based on genetic and environmental factors, particularly where an individual’s recent ancestors lived on the planet. Melanin is produced in specialized organelles called melanosomes, located within melanocytes, which make up about 1% of epidermal cells. Once synthesized, melanin is transported to surrounding keratinocytes, where it forms supranuclear “caps” that shield DNA from UV damage. The amount of melanin produced depends on how much protection the skin requires from sunlight.
Human evolution provides important context for this adaptation. The first humans, who evolved in equatorial Africa, were exposed to intense, direct sunlight throughout the day. Without clothing, houses, sunscreen, or other modern barriers to sunlight, their skin adapted to absorb and manage maximum levels of UV radiation. This led to the development of darker pigmentation, rich in melanin, to protect against excessive radiation while still allowing for adequate vitamin D synthesis.
Figure 1 from The Protective Role of Melanin Against UV Damage in Human Skin
Melanin Content in Skin of Different Ethnicity: Histological detection of melanin content using Fontana-Masson staining. Melanin content in the basal layers of the epidermis is substantially higher in Black skin compared to Asian or White skin, although the number of melanocytes is virtually identical in skins of different ethnicity.
As humans migrated to regions farther from the equator, the angle and intensity of sunlight decreased. In these environments, high levels of melanin became a disadvantage, as it inhibited UVB absorption and, consequently, vitamin D production. To survive and thrive, humans in these regions evolved fairer skin, which allowed more UVB photons to penetrate the skin and optimize vitamin D production. In essence, the evolution of lighter skin tones was nature’s way of adapting to reduced sunlight exposure, ensuring sufficient vitamin D synthesis at higher latitudes.
In modern times, migration patterns have introduced populations with varying levels of melanin to regions far from their ancestral homelands. This presents a unique challenge: individuals with higher melanin levels living in non-tropical climates, such as North America or the United Kingdom, require significantly more sunlight exposure to produce adequate vitamin D. Without this exposure, they may face a higher risk of vitamin D deficiency and associated health complications. Latitude, therefore, continues to play a critical role in vitamin D absorption, with the relationship between melanin levels, geographic location, and sun exposure remaining central to maintaining optimal health.
However, latitude and melanin are not the only factors influencing the amount of UVB radiation your skin absorbs. Altitude also plays a critical role. The higher the altitude, the shorter the distance UVB rays travel from the sun to your skin, increasing the potential for vitamin D3 synthesis. This effect has been demonstrated in studies conducted at Agra (169 meters), Kathmandu (1,400 meters), and Mount Everest Base Camp (5,300 meters), showing progressively greater vitamin D3 production with increasing altitude.
Seasonal variation further complicates the equation. The Earth’s axial tilt changes the intensity and duration of sunlight exposure throughout the year, with vitamin D levels typically dropping during colder months when the sun is less direct, and people cover their skin with more clothing to stay warm. This seasonal decline in sunlight exposure also impacts serotonin regulation, which is why individuals living farther from the equator are more prone to experiencing seasonal affective disorder (SAD) and overall poorer health outcomes during the winter.
The Clinical Benefits of Vitamin D
Often called the "sunshine vitamin," vitamin D is actually a fat-soluble steroid hormone that regulates the expression of more than 1,000 genes in the body. It plays a crucial role in immune system function and the circadian system through its influence on brain structures. Additionally, vitamin D is essential for calcium absorption, critically affecting skeletal health and cardiovascular function.
As described earlier, the biological process for synthesizing vitamin D is intricate. When sunlight hits the skin, it initiates a series of biochemical reactions, converting 7-dehydrocholesterol into previtamin D3, which is absorbed into the bloodstream via the lymphatic system. Further hydroxylations in the liver and kidneys convert it into the bioactive form of vitamin D, which is essential for calcium absorption in the intestines. Without adequate vitamin D levels, the body can only absorb 10–15% of the calcium required from food.
In their review article Vitamin D: The “Sunshine” Vitamin, researchers Rathish Nair and Arun Maseeh explain the extensive impact of vitamin D receptors (VDR), which are present in most tissues and cells in the body. They note that VDR activity influences numerous biological processes, including inhibiting cellular proliferation, inducing cell differentiation, suppressing angiogenesis, stimulating insulin production, and modulating immune responses via macrophage cathelicidin production. Additionally, sunlight enhances mitochondrial energy production—often described as the "powerhouse of the cell."
A 2014 observational study conducted in Sweden investigated sun avoidance as a risk factor for all-cause mortality. The study followed 29,518 women over 20 years and found that avoiding sun exposure was associated with a twofold increase in mortality compared to women with the highest levels of sun exposure. Remarkably, the study also reported that lifelong smokers in the highest sun exposure group had a similar risk of mortality as non-smokers who avoided the sun. This finding underscores the profound impact of sunlight on overall health—suggesting that avoiding sunlight may pose a health risk comparable to smoking.
Cancer
A review of 63 observational epidemiological studies in the PubMed database explored the relationship between vitamin D status and cancer risk. These studies examined several types of cancer, including 30 on colon cancer, 13 on breast cancer, 26 on prostate cancer, and 7 on ovarian cancer. Many of the studies also assessed associations between vitamin D receptor (VDR) genotypes and cancer risk. The majority of findings suggest a protective relationship between adequate vitamin D levels and a lower risk of cancer.
Vitamin D appears to exert its protective effects through several mechanisms. It decreases cell proliferation, promotes cell differentiation, inhibits the growth of new blood vessels (angiogenesis), and exhibits potent anti-inflammatory properties. Adequate UVB exposure has even been associated with a reduced risk of prostate cancer. Among the cancers studied, the strongest evidence supports a link between low vitamin D levels and an increased risk of colorectal cancer. Additionally, higher vitamin D intake has been associated with a lower risk of breast cancer in some studies.
While a definitive causal relationship between vitamin D and cancer has not yet been established, the evidence overwhelmingly suggests that insufficient vitamin D levels may increase the risk of developing various cancers.
Heart Disease
Vitamin D deficiency has been strongly associated with an increased risk of cardiovascular disease. Research suggests that vitamin D may protect the heart through multiple mechanisms, including modulation of the renin–angiotensin hormone system, suppression of inflammation, and direct effects on the cells of the heart and blood vessel walls.
Findings from the Framingham Heart Study revealed that individuals with low vitamin D levels had a 60% higher risk of developing heart disease compared to those with adequate levels. Additional research has linked vitamin D deficiency to a twofold increase in rates of myocardial infarction (heart attacks). One longitudinal study, which followed men and women for four years, found that individuals with low vitamin D levels were three times more likely to develop hypertension compared to those with sufficient levels.
Furthermore, the Third National Health and Nutrition Examination Survey (NHANES-III), which included 12,644 participants, demonstrated significant correlations between healthy blood pressure, pulse pressure, and adequate vitamin D levels. These findings have been further supported by studies examining the relationships between age, blood pressure, and vitamin D status, underscoring the essential role of vitamin D in maintaining cardiovascular health.
Obesity
Vitamin D deficiency is strongly correlated with obesity, and some researchers have proposed a potential causal relationship. Low vitamin D levels have been associated with unfavorable body composition metrics, including higher body mass index (BMI), increased waist circumference, and greater body fat percentage. Conversely, adequate vitamin D levels have been linked to reduced biological age and leaner body mass.
Research also indicates that vitamin D deficiency is more pronounced in individuals with higher levels of adipose tissue and lower levels of high-density lipoprotein (HDL). This effect appears to be particularly significant in individuals with higher melanin levels living at latitudes farther from the equator, where sunlight exposure is often insufficient to maintain optimal vitamin D levels.
Studies have further demonstrated that weight loss, particularly in postmenopausal overweight or obese women, is associated with an increase in vitamin D levels, highlighting the potential bidirectional relationship between vitamin D status and weight regulation. Additionally, low vitamin D levels have been strongly associated with various metabolic conditions, including insulin resistance, type 2 diabetes, hypertension, and other cardiovascular diseases, reinforcing its central role in metabolic health.
Diabetes
Research consistently shows that individuals with type 2 diabetes mellitus (T2DM) have significantly lower vitamin D levels compared to control groups. Some studies suggest that vitamin D deficiency may play a causal role in the development of T2DM, rather than simply being a correlational factor. Notably, individuals with adequate vitamin D levels have been found to have a reduced risk of developing the disease (e.g., Pittas et al., 2007, 2010, 2012; Mitri et al., 2011; Chagas et al., 2012; Lim et al., 2013).
Vitamin D also appears to play a role in glucose homeostasis. For instance, lower vitamin D levels are inversely related to glycosylated hemoglobin (HbA1c) levels in gestational diabetes mellitus, suggesting a direct impact on blood sugar regulation.
In addition to vitamin D’s role, modern lifestyle factors like blue light exposure—commonly emitted from electronic devices—have been shown to impair glucose tolerance and increase sugar cravings. This research underscores a dual concern: vitamin D deficiency due to insufficient sun exposure may contribute to diabetes pathophysiology, while negative light exposure from modern devices could exacerbate glucose dysregulation.
Depression
A Norwegian randomized, double-blind trial demonstrated that overweight participants receiving high-dose vitamin D supplementation (20,000 or 40,000 IU weekly) experienced significant improvements in depressive symptoms compared to those receiving a placebo. This study underscores a strong correlation between vitamin D levels and the risk of depression.
Vitamin D, a neuroactive steroid, has been shown to increase dopamine, tyrosine, and serotonin levels in the brain—key neurotransmitters that play critical roles in regulating mood. Furthermore, a meta-analysis revealed that bright light therapy and sun exposure were associated with significant reductions in depression symptoms. These interventions were effective for both seasonal affective disorder (SAD) and nonseasonal depression.
Other studies have observed a dose-response relationship between sunlight exposure and mood, showing that greater sunlight exposure is consistently linked to improved emotional well-being. This evidence highlights the importance of both adequate vitamin D levels and natural light exposure in promoting mental health.
Cognitive Impairment
The Italian Chianti population-based study (InCHIANTI) revealed that low levels of vitamin D are associated with significant cognitive decline in elderly individuals over a six-year period. Notably, this decline appeared most pronounced in executive functioning, whereas memory and other cognitive domains were comparatively less affected.
Sunlight exposure has also been linked to increased production of orexin (hypocretin), a neuropeptide involved in regulating critical homeostatic functions, including the sleep/wake cycle, energy balance, food intake, and arousal. Furthermore, seasonal variations in sunlight exposure have been positively correlated with concentrations of Brain-Derived Neurotrophic Factor (BDNF), a key molecule in brain plasticity that supports learning and memory.
Low vitamin D levels have also been identified as a significant risk factor for dementia and Alzheimer’s disease. Additionally, research suggests that vitamin D may have neuroprotective effects, potentially reducing the risk of developing multiple sclerosis (MS) and other neurological disorders. These findings underscore the essential role of vitamin D and sunlight exposure in maintaining cognitive health and preventing neurological decline.
Alzheimer’s Disease
A 2014 study examined 1,658 Americans aged 65 and older who were free of dementia and capable of walking unaided at baseline. Over a six-year follow-up period, the investigators found a striking correlation between vitamin D deficiency and the development of Alzheimer’s disease. Participants with vitamin D levels below 10 ng/mL were twice as likely to develop Alzheimer’s compared to those with adequate levels of vitamin D.
Parkinson’s Disease
Emerging research suggests that chronic vitamin D deficiency may significantly contribute to the development of Parkinson’s disease. A cohort study based on the Mini-Finland Health Survey found that low vitamin D levels could potentially predict the onset of Parkinson’s. Additionally, other studies indicate that maintaining adequate vitamin D levels may help reduce the risk of developing this neurodegenerative condition.
Psoriasis
A 2012 study found that individuals with psoriasis were more likely to have low vitamin D levels. The investigators highlighted that both sun exposure and vitamin D derivatives, such as topical treatments, are commonly utilized in managing psoriasis, suggesting a potential therapeutic role for optimizing vitamin D levels in patients with this condition.
Pregnancy
Obstetric endocrinology has highlighted the critical role of vitamin D in supporting both maternal and fetal health during pregnancy. Vitamin D requirements increase significantly, particularly during the third trimester, to meet the demands of fetal development and maternal well-being. Poor maternal vitamin D levels during pregnancy have been linked to various complications in infants, including rickets, osteomalacia, metabolic disorders, and bone development issues.
For mothers, vitamin D deficiency has been associated with pregnancy-induced hypertension, gestational diabetes mellitus, recurrent pregnancy loss, preterm delivery, primary Caesarean section, and postpartum depression. Additionally, an analysis of data from the National Health and Nutrition Examination Survey (NHANES) found that pregnant women with low vitamin D levels were nearly three times more likely to develop bacterial vaginosis (BV), further emphasizing the importance of maintaining adequate vitamin D levels during pregnancy.
Bone Fractures and Falls
Vitamin D is essential for maintaining bone health, primarily by facilitating the absorption of calcium. Beyond its role in bone density, vitamin D is also theorized to enhance muscle strength, particularly through its interaction with receptors on fast-twitch muscle fibers, which may help prevent falls.
A meta-analysis of 12 fracture-prevention trials demonstrated that supplementation with approximately 800 IU of vitamin D daily reduced the risk of hip and nonspinal fractures by about 20%. Supporting these findings, researchers at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University reviewed trials comparing vitamin D supplementation to placebo for fall prevention. They concluded that "fall risk reduction begins at 700 IU and increases progressively with higher doses." These findings emphasize the importance of adequate vitamin D intake for reducing fracture and fall risks, particularly in older adults.
Autoimmune Diseases
Vitamin D's immunomodulatory, anti-inflammatory, antioxidant, and anti-fibrotic properties have drawn significant attention from researchers exploring its role in the pathophysiology of autoimmune diseases.
A comprehensive 2019 literature review of over 130 studies revealed a strong association between low vitamin D levels and several autoimmune conditions. These included systemic lupus erythematosus (SLE), thyrotoxicosis, type 1 diabetes mellitus (DM), multiple sclerosis (MS), iridocyclitis, Crohn’s disease, ulcerative colitis, psoriasis vulgaris, seropositive rheumatoid arthritis (RA), and polymyalgia rheumatica.
These findings highlight the potential importance of maintaining adequate vitamin D levels as part of managing or mitigating the risk of autoimmune disorders, though more research is needed to clarify causal mechanisms and therapeutic implications.
Liver Disease
A 2015 review highlighted the potential of sun exposure to mitigate the development of non-alcoholic fatty liver disease (NAFLD). The study found an inverse association between sun exposure and NAFLD, suggesting that sunlight may play a protective role in preventing liver inflammation.
These findings indicate that sunlight, likely through its role in vitamin D synthesis and associated anti-inflammatory pathways, could contribute to liver health. However, further research is needed to elucidate the precise mechanisms and therapeutic potential of sunlight in preventing or managing liver disease.
Influenza
Vitamin D deficiency may be a seasonal trigger for winter influenza outbreaks. A randomized controlled trial in Japan found that children taking a daily 1200 IU vitamin D supplement had a 40% lower rate of influenza type A compared to those on a placebo, highlighting the potential protective role of adequate vitamin D levels.
Pelvic Floor Disorders
Pelvic floor disorders, including urinary and fecal incontinence, increase with age and are often linked to osteoporosis and low bone mineral density. A review of the National Health and Nutrition Examination Survey revealed that women with lower vitamin D levels are at higher risk for pelvic floor disorders. Additionally, women over 50 with suboptimal vitamin D levels were found to have a greater likelihood of urinary incontinence.
Statin intolerance
A 2015 study found that vitamin D supplementation can effectively resolve statin intolerance caused by myalgia, myositis, myopathy, or myonecrosis. The authors also suggested that sun exposure might play a role in addressing vitamin D deficiency in these patients
Macular Degeneration
Aging
Research has indicated that a vitamin D deficiency can accelerate aging and age-related disease, by promoting autophagy, decreasing inflammation, optimizing mitochondria, decreasing oxidative stress, enhancing Ca2+ in the brain, promoting a positive epigenetic expression, and helping to maintain telomere length. Other studies have confirmed that vitamin D deficiency plays a pivotal role in mitochondrial dysfunction, which has be associated with premature aging. In a study of over 2,000 women, those with optimal vitamin D levels had longer telomeres—a key biomarker of biological age—while those with deficiencies had shorter telomeres, reflecting accelerated aging.
Tooth Decay
Vitamin D deficiency has been linked to increased rates of periodontitis, gingival inflammation, tooth decay, dental caries, and a variety of other oral health disorders. Optimal vitamin D levels support oral health by promoting calcium absorption, which strengthens teeth and helps maintain healthy gums.
All-cause mortality
A 2014 meta-analysis analyzing data from 73 cohort studies (849,000 participants) and 22 randomized controlled trials (31,000 participants) found that low vitamin D levels significantly increased the risk of cardiovascular diseases, cancer, and other causes of death (RR 1.35, 95% CI 1.22–1.49 for all-cause mortality when comparing the lowest third to the top two-thirds of circulating 25(OH)D levels). The authors estimated that 9.4% of all deaths in Europe and 12.8% in the United States could be directly attributed to vitamin D insufficiency.
Similarly, a 2016 meta-analysis of 32 studies (30 cohort studies and 2 nested case-control studies) found that individuals with the lowest vitamin D levels had nearly twice the mortality rate of those with the highest levels of vitamin D.
Additionally, a 2014 study following 29,518 Swedish women over 20 years found that habitually avoiding the sun increased the risk of all-cause mortality by 40%, further emphasizing the critical role of vitamin D and sun exposure in overall health and longevity.
Vitamin D & the Immune System
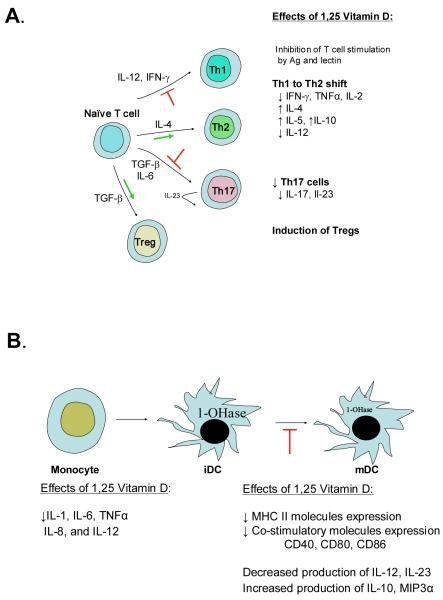
Figure 1 from Vitamin D and the Immune System
A. Effects of 1,25 Vitamin D on T cells include suppression of T cell proliferation, a shift from Th1 to a Th2 development, inhibition of Th17 cell development and facilitation of T regulatory cells. B. Effects of 1,25 Vitamin D on monocytes and dendric cells include inhibition of inflammatory cytokine production by monocytes and inhibition of dendritic cell differentiation and maturation.
Emerging evidence highlights vitamin D as a primary modulator of the immune system. Historically, heliotherapy—exposure to sunlight—was used to treat infections like tuberculosis before antibiotics were available. Tuberculosis patients were sent to sanatoriums to receive sunlight exposure, believed at the time to "kill the tuberculosis." While we now understand that sunlight alone doesn’t directly kill bacteria, it facilitates immune responses by enhancing vitamin D levels, which play a critical role in immune regulation.
Numerous studies link low vitamin D levels with an increased risk of infection. For instance, a study of nearly 19,000 individuals (1988–1994) found that those with lower vitamin D levels were significantly more likely to develop upper respiratory tract infections, even after adjusting for factors such as season, age, gender, body mass, and race. Similar associations have been observed between vitamin D levels and conditions such as influenza, bacterial vaginosis, and even HIV.
The biological mechanisms underpinning the connection between vitamin D and immunity are becoming clearer. T lymphocytes, crucial players in immune responses, appear to be photosensitive, with sunlight enhancing their mobility and functionality. Additionally, vitamin D:
Inhibits B cell proliferation and blocks their differentiation and immunoglobulin secretion.
Suppresses T cell proliferation, shifting immune responses from an inflammatory Th1 to an anti-inflammatory Th2 phenotype.
Facilitates the maturation of T regulatory cells while reducing pro-inflammatory Th17 responses.
Decreases inflammatory cytokine production (e.g., IL-17, IL-21) while promoting anti-inflammatory cytokines like IL-10.
Influences monocytes and dendritic cells by inhibiting the production of inflammatory cytokines (e.g., IL-1, IL-6, IL-8, IL-12, TNFα) and preserving an immature dendritic cell phenotype. This is marked by reduced expression of MHC class II molecules and co-stimulatory signals.
This burgeoning field, referred to as "photoimmunology," continues to explore the intricate interplay between sunlight and the immune system. What is already evident is that sunlight, through its role in vitamin D synthesis, is a key contributor to the delicate balance required for optimal immune function.
Patients at the Jewish Consumptives’ Relief Society (circa 1930) participated in heliotherapy, or sun exposure, as treatment for tuberculosis. Photo courtesy of Beck Archives, University of Denver.
Sunlight & Circadian Rhythm
Electronically published by the Brain Treatment Center of Asia ("Circadian Rhythm").
The human body operates on a set of circadian rhythms—a 24-hour internal clock—closely tied to the cycle of sunrise and sunset. These rhythms influence nearly every biological function. When light enters your eyes, photoreceptors in rods, cones, and melanopsin-expressing retinal ganglion cells convert the light into electrical signals. These signals travel along the optic nerve to the hypothalamus, which houses the suprachiasmatic nucleus (SCN), a structure of about 20,000 neurons responsible for regulating your circadian rhythm.
The SCN controls melatonin, the hormone central to sleep regulation and circadian synchronization. In the morning, exposure to natural blue light reduces melatonin production, promoting wakefulness. As daylight fades and red wavelengths dominate, melatonin levels rise, signaling that it’s time for sleep. Beyond sleep, melatonin supports mitochondrial repair and synchronization of peripheral cellular clocks. It also enhances innate immunity, complementing sunlight’s activation of T-cells.
However, excessive exposure to artificial blue light—such as from TVs, phones, or computers—can disrupt this natural process. Studies show that even minimal light exposure at night, like a streetlamp outside a window, can suppress melatonin by 85%. Wearing blue-light-blocking glasses during nighttime can mitigate this effect, as shown by research from the University of Toronto. Blue light also suppresses delta brainwaves, which promote deep sleep, while amplifying alpha brainwaves, associated with alertness, further disrupting rest.
Neuroscientist Andrew Huberman, PhD, from Stanford University, emphasizes the adverse effects of bright light exposure between 11:00 PM and 4:00 AM. Bright light during these hours triggers depressive circuits in the habenula, a structure in the thalamus. The habenula connects to the pancreas, influencing blood sugar regulation. Bright light exposure can elevate blood sugar levels and reduce insulin sensitivity, which may have long-term metabolic consequences.
Moreover, the body’s sensitivity to light varies by time of day. Around 4:00 AM, UV light naturally reduces adrenaline production and triggers cortisol release, helping the body transition from rest to wakefulness. This process involves water flow between glial cells and neurons through aquaporin 4 gates, supporting natural waking processes.
A 2019 study published by the Society for the Study of Ingestive Behavior found that negative blue light exposure disrupted the body’s ability to regulate blood sugar and insulin, potentially contributing to obesity and diabetes. The researchers concluded that light exposure can be as critical as nutrition for metabolic health. Even a perfect diet may be undermined by poor light hygiene, underscoring the need for mindful light exposure to optimize health.
What About Vitamin D Supplements?
While synthetic vitamin D supplements can help address deficiencies, they are not equivalent to vitamin D synthesized naturally through sun exposure. Sunlight triggers the production of nearly 1,000 photochemicals in the plasma alongside the active forms of vitamin D3, whereas supplements predominantly provide vitamin D2. Furthermore, excessive supplementation can disrupt your body’s ability to synthesize vitamin D3 naturally. Unlike sunlight, which has a built-in mechanism to prevent toxicity, synthetic supplements can lead to vitamin D toxicity if consumed in excessive amounts. Studies have also demonstrated that vitamin D derived from sunlight has a more significant impact on bone health and calcium regulation than synthetic alternatives.
The Natural Forms of Vitamin D:
Vitamin D1: A molecular compound of ergocalciferol (D2) and lumisterol in a 1:1 ratio.
Vitamin D2 (Ergocalciferol): Produced by invertebrates, some plants, and fungi, with production stimulated by ultraviolet light.
Vitamin D3 (Cholecalciferol): Synthesized in the skin when UVB radiation reacts with 7-dehydrocholesterol.
Vitamin D4: An analog scientifically referred to as 22-dihydroergocalciferol.
Vitamin D5 (Sitocalciferol): An analog synthesized from 7-dehydrositosterol.
The Synthetic Forms of Vitamin D:
Maxacalcitol (22-oxacalcitriol or OCT): Known for its wider therapeutic window compared to natural vitamin D.
Calcipotriol: A calcitriol derivative, initially used in trials for osteoporosis treatment.
Dihydrotachysterol (DHT): A synthetic form that activates in the liver without requiring kidney hydroxylation, making it advantageous for some conditions.
Paricalcitol (19-norD2): Used for secondary hyperparathyroidism and distinct from calcitriol due to its altered side chain.
Tacalcitol: A derivative of vitamin D3 that inhibits keratinocyte proliferation in the skin.
Doxercalciferol (1α(OH)D2): A prodrug that becomes active in the body and is less toxic than its D3 counterpart when used chronically.
Falecalcitriol (1,25(OH)2-26,27-F6-D3): Approved in Japan for secondary hyperparathyroidism and more active due to slower metabolism.
Rickets and the Discovery of Vitamin D
Dr. Theobald Palm
In the 1600s, as the Industrial Revolution swept through Europe, cities became more crowded, and coal-burning led to unprecedented air pollution. Around the same time, a bone-deforming disease called rickets began appearing in children at alarming rates.
The first scientist to connect the rise of industrialization with rickets was a Polish physician, Jędrzej Śniadecki, in 1822. Śniadecki observed significantly higher rates of rickets among children in inner-city Warsaw compared to those in rural areas.
In the 1880s, Scottish doctor and missionary Theobald Palm expanded on these observations, theorizing a link between sunlight exposure and rickets. Analyzing an epidemiologic map published by the British Medical Association in 1889, Palm noted that rickets was most prevalent in large towns and densely populated districts. Drawing on his travels to Tokyo and other equatorial regions where rickets was uncommon, Palm developed the idea of "sunshine as a means of health." Despite his insights, his theory was largely dismissed at the time.
Nearly 100 years after Śniadecki's work, German pediatrician Kurt Huldschinsky demonstrated in the early 20th century that exposing children with rickets to a mercury arc lamp significantly improved their condition within months. He was the first to hypothesize that sunlight stimulated the production of a critical substance in the skin necessary for bone health.
In 1921, American physicians Alfred F. Hess and Lester J. Unger published the first case study demonstrating that exposing children with rickets to sunlight could cure the disease. Conducting their research on the rooftop of a New York City hospital, they noted that children with darker skin, who were disproportionately affected by rickets, required more time in the sun to achieve the same therapeutic benefits.
Around the same period, scientists Harry Steenbock and Archie Black began experimenting with fortifying foods by exposing them to UV light. They discovered that adding a fungal sterol, ergosterol, to milk and irradiating it with UVB light produced vitamin D2. By 1931, this practice became widespread in the dairy industry in the United States and the United Kingdom. Government campaigns promoting milk consumption for stronger bones followed, and within a few years, this innovation effectively eradicated rickets in many parts of the world.
However, by the 1940s, the enthusiasm for vitamin D fortification spiraled out of control as food manufacturers began adding vitamin D to a wide array of products to market them as "healthy." By the 1950s, this excessive fortification led to an alarming outbreak of hypercalcemia in infants, a condition characterized by dangerously high calcium levels. Symptoms included distinctive "elfin-shaped" faces, heart problems, and developmental delays.
An investigation by the Royal College of Physicians traced the issue to vitamin D toxicity caused by the over-fortification of foods. In response, many countries reevaluated and restricted which foods could be fortified with vitamin D.
Figure 5. from Sunlight and Vitamin D
Photographs of researchers who made crucial contributions to vitamin D and rickets research. (A) Jędrzej Śniadecki, (B) Kurt Huldschinsky, (C) Alfred Hess, (D) Harry Steenbock. Holick, copyright 2013. Reproduced with permission.
Figure 6. from Sunlight and Vitamin D
UV radiation therapy for rickets. (A) Photograph from the 1920s of a child with rickets being exposed to UV radiation. (B) Radiographs demonstrating florid rickets of the hand and wrist (left) and the same wrist and hand taken after treatment with 1 h UV radiation 2 times a week for 8 weeks. Note mineralization of the carpal bones and epiphyseal plates (right). Holick, copyright 2006. Reproduced with permission.
Figure 7. from Sunlight and Vitamin D
(A) Seal of a milk bottle that denoted that the milk was irradiated with UV radiation and contained vitamin D. (B) Cap of a milk bottle stating that activated ergosterol has been added to the milk. (C) Cap of milk bottle stating that the milk had been fortified with vitamin D. (D) Seal of a bottle of milk that denoted that the milk had been irradiated and contained vitamin D. Holick, copyright 2013. Reproduced with permission.
Figure 9. from Sunlight and Vitamin D
(A) Seal denoting that this product was fortified with vitamin D. (B) Bottle of oil denoting that it contained irradiated ergosterol. (C) Beer can denoting that it was fortified with vitamin D. (D) Advertisement denoting that Bird’s custard contained vitamin D. Holick, copyright 2013. Reproduced with permission.
The Rarely Seen History of Light Therapy
Niels Ryberg Finsen, December 15, 1860, Thorshavn, Faroe Islands; + 24 September 1904; Nobel Prize was awarded “in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science.”
The therapeutic use of light can be traced back to the late 19th century when Danish researcher Niels Ryberg Finsen demonstrated that light could stimulate the immune system to combat infections. His pioneering artificial light device, known as the "Finsen lamp," laid the groundwork for modern phototherapy.
Light therapy developed along two primary lines: heliotherapy (natural sun therapy) and phototherapy (artificial light therapy). During the early 20th century, heliotherapy gained widespread popularity, particularly in Europe, as a treatment for chronic illnesses such as tuberculosis and lupus. In northern latitudes, heliotherapy remains practiced today in some areas.
Dr. Auguste Rollier was one of heliotherapy’s most influential practitioners. He established a renowned sun-therapy clinic in Leysin, located in the Swiss Alps. Patients with various conditions were treated by being exposed to sunlight for prescribed periods daily, often on large sundecks designed for this purpose. Unfortunately, heliotherapy began to decline in the mid-20th century with the increasing reliance on pharmaceutical drugs, particularly in the United States.
In the 1930s, Charing Cross Hospital in London integrated “sun-lamps” into its treatments, using artificial UV light for conditions such as circulatory diseases, anemia, varicose veins, heart disease, and degenerative disorders.
The 1940s marked a significant advancement in phototherapy with the invention of the Knott Hemo-Irradiator by Emmitt Knott. This device irradiated a small volume of blood (50–100cc) with ultraviolet light, which was then reintroduced into the patient. It demonstrated remarkable success in treating infections and conditions such as puerperal sepsis, peritonitis, encephalitis, polio, and herpes simplex, with reported success rates between 50% and 80%. By 1947, over 80,000 patients had received treatment with the Knott Hemo-Irradiator. However, concerns arose regarding the potential cancer risks of prolonged radiation exposure, leading to its decline in use.
Interestingly, modern advancements in light therapy have rekindled interest in Knott’s work. Intravenous laser blood irradiation, a contemporary variation of his original device, is now being used in clinics worldwide. Recent studies are promising and aim to establish the safety and efficacy of this renewed approach to light-based treatments.
Intravenous Laser Therapy being performed by The New York Center for Innovative Medicine (NYCIM).
Gallery of historical light therapies compliments of Rare Historical Photos.
The Modern World
Between 1850 and 1860, English chemist Joseph Swan developed the world’s first light bulb using carbonized paper filaments. By 1878, he was awarded a patent for his invention in the United Kingdom. Among the many intrigued observers was American inventor Thomas Edison, who noted a flaw in Swan's design: it required too much electricity. In 1879, Edison patented his improved version of the light bulb in the U.S. and Canada, using a carbonized bamboo filament that could burn for more than 1,200 hours. This innovation laid the foundation for modern artificial lighting, transforming human exposure to light overnight.
Until then, humans had only been exposed to natural sunlight and firelight. General Electric then helped slingshot the advancement of light bulbs over the next century; first with a physicist named William David Coolidge, who began using tungsten filaments, and then later Nick Holonyak, who accidentally invented the red LED light for the company while trying to create a laser. Subsequently, yellow and green LEDs were added to the mix and then eventually the blue LED, created in the early 1990’s by Isamu Akasaki, Hiroshi Amano, and Shuji Nakamura, a group of Japanese and American scientists, for which they won the 2014 Nobel Prize in Physics. It only took a little more than 100 years and humans went from only natural sunlight to blue LED lights being used everyday. However, this leap forward has raised important questions: Are there long-term health implications of modern artificial lighting?
Sir William Crookes - 1906
In nature, sunlight emits the full light spectrum, balancing blue light's stimulation with red light's calming and regenerative effects. Modern devices like smartphones, TVs, and computers rely heavily on blue light, which is cheaper to produce and more energy-efficient than full-spectrum light. Unfortunately, this cost-driven decision disregards the human body's biological dependence on balanced light exposure.
Similarly, tools to block natural light, like sunglasses, are relatively new inventions. In 1913, British chemist Sir William Crookes created UV-blocking lenses for patients with syphilis, a condition causing extreme light sensitivity. By 1929, sunglasses became a fashion accessory, mass-produced by Sam Foster in the U.S. However, the unintended consequence of sunglasses is reduced natural light exposure, which may carry health risks. Dr. Albert Schweitzer, working in Lambarene, Africa, observed an increase in cancer cases after the introduction of sunglasses, theorizing that reduced sunlight exposure to the retina could play a role. Supporting this, a JAMA Neurology study found that blue light exposure and thinner retinal nerve fiber layers (RNFL) were associated with increased cognitive decline.
The use of sunscreen also has a fascinating history. Ancient civilizations like the Greeks and Indians used zinc oxide as a skin protectant. Modern sunscreen wasn’t introduced until 1928, with the French chemist Eugène Schueller, founder of L’Oreal. It became widely popular in 1944, when airman and pharmacist Benjamin Green developed a sunscreen for U.S. soldiers stationed in tropical climates. Commercial brands like Coppertone capitalized on its popularity, promoting it as a beauty product rather than a health necessity.
While sunscreen is often recommended for skin cancer prevention, recent research challenges its efficacy. A meta-analysis of 29 studies involving over 313,000 participants found no significant correlation between sunscreen use and reduced skin cancer risk. Instead, many sunscreens block the body's ability to produce vitamin D, a deficiency linked to several chronic diseases. Furthermore, many sunscreens contain toxic chemicals, with only 21% meeting safety thresholds set by the Environmental Working Group (EWG). Ingredients like oxybenzone, avobenzone, and retinyl palmitate should be avoided due to potential neurotoxic effects.
For safer alternatives, consider sunscreens containing only zinc oxide or titanium dioxide without additives. Additionally, dietary antioxidants like astaxanthin, omega-3 fatty acids, vitamin E, and beta-carotene can naturally protect the skin. Protective clothing and hats are also effective measures for minimizing harmful UV exposure.
Sunburns & Skin Cancer
Types of skin cancer, photo compliments of the Mayo Clinic.
Skin cancer rates have surged over the past 50 years. While some attribute this to increased UVB exposure due to ozone depletion, others suggest that lifestyle changes, such as more time spent outdoors and inadequate sun protection, are contributing factors.
A sunburn is not a thermal burn caused by heat but is instead a biological response to UV radiation. Keratinocytes, the primary cells in the epidermis, play a central role in this process. When UVB rays are absorbed by chromophores within the cells, such as genomic DNA, a biochemical response is triggered. This process is crucial for beneficial effects like converting 7-dehydrocholesterol to previtamin D. However, excessive UVB exposure can lead to DNA damage or damage to other chromophores in keratinocytes.
If this damage surpasses the cell's repair capacity, the keratinocytes undergo apoptosis (programmed cell death). The characteristic redness and pain of a sunburn are due to inflammation and vasodilation associated with this process. The balance between cell survival and apoptogenic factors is delicate, and chronic UVB stress can disrupt this balance, contributing to carcinogenesis.
Skin cancer has been linked to mutations in key tumor suppressor genes, particularly the p53 gene, often referred to as the "guardian of the genome." This gene is vital for repairing DNA damage and eliminating irreparably damaged cells. Chronic UVB stress can cause mutations in p53, leading to the survival and replication of cells with severe DNA damage. This process underpins the development of skin cancers like basal cell carcinoma and squamous cell carcinoma. Unique p53 mutations have been observed in UV-induced skin cancers, distinguishing them from other cancer types.
The relationship between sun exposure and melanoma remains complex. While excessive UV exposure is a known risk factor, vitamin D may offer protective benefits against certain skin cancers. However, studies investigating this link have yielded conflicting results, and more research is needed to fully understand the interplay between vitamin D, sun exposure, and skin cancer risk. The paradox of increasing sunscreen use and rising skin cancer rates raises questions about the effectiveness of modern sun-protective strategies. It suggests that while tools like sunscreen reduce UV exposure, other factors—such as improper application, inadequate coverage, or reliance on chemical-based products—may undermine their efficacy.
Emerging research suggests that fasting or calorie-restriction diets may provide protective effects against skin cancer by promoting apoptosis and modulating epithelial growth factors. This aligns with evolutionary theories proposing that intermittent fasting, common among early humans due to food scarcity, may have conferred a degree of natural resilience to UV damage.
Sugar consumption has been linked to the formation of advanced glycation end-products (AGEs), which accelerate the aging of connective and vascular tissues. Excessive AGEs may exacerbate the harmful effects of UV radiation on the skin. Conversely, proanthocyanidins, found in foods like berries and grape seeds, have demonstrated potential for protecting DNA from UV-induced mutations, offering another dietary avenue for mitigating sun damage.
Photo of the four main types of skin cancers, from SurgMedia.